THE VIRTUAL PANEL SESSION TO MARK WORLD SICKLE CELL DAY 2025

World Sickle Cell Day 2025 – Access to New Therapies: Hope or Hype?
June 11, 2025
Nourishing Red Blood Cells: Why Folic Acid-Rich Foods Are Essential for Children with Sickle Cell Disease
July 22, 2025
THE VIRTUAL PANEL SESSION TO MARK WORLD SICKLE CELL DAY 2025 HELD ON 12TH JUNE 2025
THEME: ACCESS TO NEW THERAPIES: HYPE OR HOPE?
The National Director and CEO of the Sickle Cell Foundation Nigeria (SCFN), Dr. Annette Akinsete, gave the welcome address. In her opening remarks she dwelt on growing concerns about equity and access to new therapies in low-resource settings. She also stated that innovation without equity is inadequate and gives rise to injustice in the health sector. She then called on governments, the private sector and international organisations to take notice and take action. Her opening speech was followed by the address of the Chairman, Board of SCFN, Chief Tunde Afolabi (MFR). His speech, which was delivered by Mrs. Uwa Ohiku, a member of the SCFN Board, addressed the urgent need to bridge the widening gap between scientific breakthroughs and equitable access. While declaring the panel session open, he said that ensuring equitable access to new therapies must become a shared priority. In his words: “It’s a call to reflection and a call to action.”
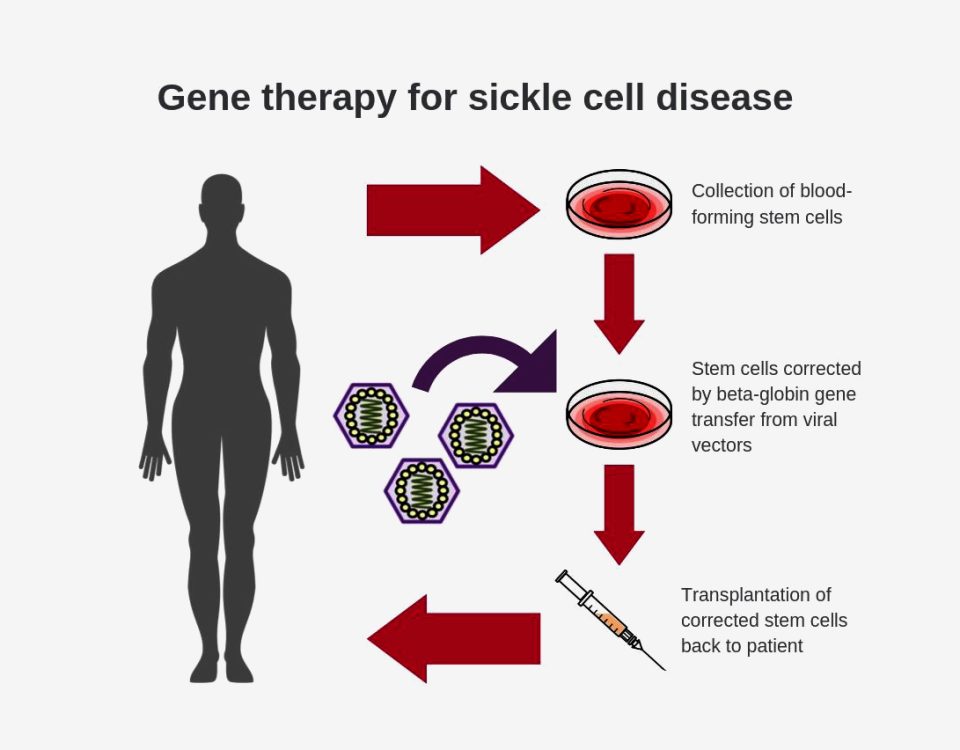
Prof. Julie Makani gave the keynote address on Advanced Therapy for Sickle Cell Disease in Africa: Blood Transfusion, Bone Marrow Transplant and Pathway to Gene and Cell Therapy. In her address, she raised the issue of whether public health interventions or curative health should be prioritised considering the current limitations of accessing new therapies. In her opinion both should be prioritised with different groups of people addressing one or the other. She also raised concerns about gene therapy trials being limited to the developed world considering that the greater number of people living with SCD reside in Africa. She said that there was no reason for Africa to be left out of trials, especially as it was important to find out what works for different patients in various parts of the world. She concluded by saying that these trials can be done through partnerships with governments, the private sector and international agencies.
The panel discussion moderated by Dr. Titilope Fasipe probed further into the equity of BMT, gene therapies and the importance of conducting trials in Africa. Responding to the issue of trials, Prof. Adekunle Adekile explained that it was crucial to have trials in Africa because there is so much variation in genetics and that if the different types of patients are not included in trials, it may not be possible to catch the different adverse effects of therapies. He added that it was crucial to understand the pattern among patients in order to design good clinical trials. Prof. Akinola buttressed the point about variations in genetics and the need to carry out more investigations in this direction. He also drew attention to the fact that not all patients feel the need to have a transplant or gene therapy particularly if their condition is being effectively managed with Hydroxyurea. On the issue of equity and access to new therapies, Prof. Bazuaye, who pioneered BMT in the country, stated that the high reliance on foreign drugs and materials for transplants was a huge impediment to improving access in low-resource settings. Dr. Adeseye Akinsete, in his own intervention, argued that the way to bring down the cost of BMT and make it more accessible was to strengthen the local support structure by enabling the production of materials and drugs in the country. He also urged all stakeholders to come together to fashion out a way forward. Prof. Funmi Olopade also lent her voice to the call to action, urging government to support the stakeholders in providing care for those with SCD just as was being done in the United Kingdom where the government recently announced that the gene therapy would be available annually on the NHS for 50 patients with SCD. Dr. Gaurav Kharya shared his experience of BMT and explained that therapies were more affordable in India because many of the drugs required for transplants are produced there. He also talked about the challenges of transplants and advised on starting off with a clear set of indicators for transplants. He said that a transplant was likely to have a better outcome if the patient was in the early stages of SCD. He also added that once there is organ failure, it becomes more difficult to achieve success. His view is that it is better to select patients with good prognosis. He also stated that he had done 200 transplants with different outcomes and achieved a success rate of 85%. Dr. Wellington expressed the view that while work is ongoing on technology transfer and training on the new therapies, existing therapies such as Hydroxyurea, blood transfusions, and vaccinations should be used to maximum effect. She also mentioned that health insurance was now available for everyone in Lagos State and that this would go a long way to help those living with SCD. Dame Edith Okowa, in her own contribution, reported that there was some skepticism among patients with SCD about the new therapies and appealed to those patients who had successfully undergone transplants to come to seminars to give testimonies.
A number of organisations gave goodwill messages. Among those who presented goodwill messages were Dancid (represented by Prof. Kunle Adekile), Sickle Cell Support Society of Nigeria (represented by Prof. Norah Akinola), Coalition of Sickle Cell NGOs (represented by Timi Edwin), Non Communicable Diseases Alliance (represented by Prof. Kingsley Akinroye), WHO office in Nigeria (represented by Dr. Mary Dewan) and the Lagos State Ministry of Health (represented by Dr. Abosede Wellington).
The virtual panel discussion was attended online by over 400 participants from Tanzania, Kenya, Egypt, the United Kingdom, India, Nigeria, Zambia, Senegal, Cameroon, Ghana, Ireland, and the United States of America.